Do People With Rheumatoid Arthritis Have an Increased Risk of Sleep Apnea?
By Carol Eustice | Reviewed by a board-certified physician
Updated January 27, 2017
Sleep disorders are prevalent among people who have rheumatoid arthritis. Fatigue is recognized as a huge problem for those living with the disease. At one time, it was said to be unclear if obstructive sleep apnea was associated with rheumatoid arthritis. Obstructive sleep apnea is one of three types of sleep apnea.
What’s the current thinking? Is there a higher risk of developing obstructive sleep apnea if you have rheumatoid arthritis?
Is obstructive sleep apnea the cause of sleep disturbance and fatigue which are common complaints of people with rheumatoid arthritis? Let’s consider what researchers have determined.
What Is Rheumatoid Arthritis?
Rheumatoid arthritis is a chronic, autoimmune, inflammatory type of arthritis. While symmetric joint pain and joint damage are characteristic of rheumatoid arthritis, there may be systemic effects and extracurricular manifestations as well. About 1.5 million people in the United States have rheumatoid arthritis, according to the Centers for Disease Control and Prevention (CDC).
What Is Sleep Apnea?
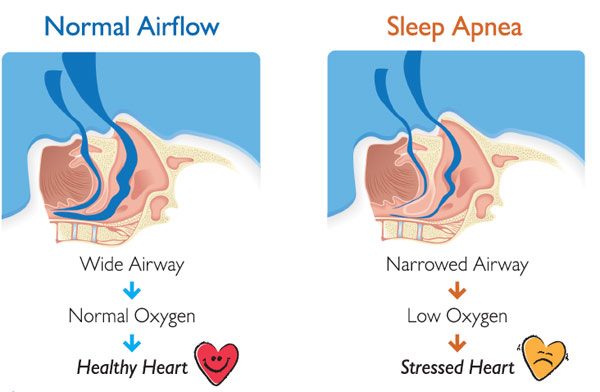
Sleep apnea is the most common sleep-related breathing disorder. With sleep apnea, a person’s breathing is interrupted or essentially stops, during sleep. In North America, the estimated prevalence—when obstructive sleep apnea is defined as apnea-hypopnea index (AHI) of greater than 5 events per hour as determined by polysomnogram—is 20 to 30 percent in males and 10 to 15 percent among females.
While apnea refers to the temporary suspension of breathing, hypopnea refers to slow or shallow breathing. Episodes of sleep apnea result in reduced oxygen saturation.
Risk factors associated with sleep apnea include:
- Advancing age
- Male gender
- Obesity
- Craniofacial or upper airway soft tissue abnormalities
Other risk factors that have been identified include smoking, nasal congestion, menopause, and family history of sleep apnea. Certain medical conditions have been linked to a higher rate of sleep apnea, including pregnancy, end-stage renal disease, congestive heart failure, chronic lung disease, and stroke. Researchers have also found a link between rheumatoid arthritis and an increased risk of obstructive sleep apnea.
How Are Sleep Apnea and Rheumatoid Arthritis Connected?
According to study results published in BMJ Open (2016), the overall incidence rate of obstructive sleep apnea was 75 percent higher in the cohort of people with rheumatoid arthritis compared to those without rheumatoid arthritis. The findings were derived from the first retrospective cohort study that utilized nationwide population-based data. Previous studies of sleep apnea and its possible association with rheumatoid arthritis were based on case reports or case studies with small sample size.
The BMJ Open study discussion states that the risk of obstructive sleep apnea is greater in men than women, in older people compared to younger people, and in those with comorbidity. The risk of sleep apnea is known to be associated with hypertension, hyperlipidemia, ischemic heart disease, and obesity.
With regard to rheumatoid arthritis, certain factors appear to contribute to the higher risk of sleep apnea, including micrognathia, cervical spine abnormalities, involvement of the temporomandibular joint, the involvement of the cricoarytenoid joint, and obesity.
- Micrognathia is a condition where the lower jaw is smaller than normal. This is often characteristic of juvenile idiopathic arthritis. It also can occur as adult-acquired micrognathia associated with rheumatoid arthritis, in some cases due to destruction of the temporomandibular joint, leading to obstruction of the upper airway and obstructive sleep apnea.
- Cervical spine issues can occur with rheumatoid arthritis, specifically, instability of the occipital-cervical junction, misalignment of the occipital-cervical region, as well as other abnormalities, such as the presence of osteophytes. Cervical misalignment can cause upper airway narrowing, brainstem compression, and can affect the severity of sleep apnea. Occipital-cervical (surgical) fusion may help to correct that particular abnormality and improve sleep apnea.
- Temporomandibular joint involvement—Destruction of the temporomandibular joint related to rheumatoid arthritis can reduce the size of the upper airway and contribute to sleep apnea in those who are affected.
- Cricoarytenoid joint involvement—The cricoarytenoid joints are located between the cricoid and paired arytenoid cartilages in the back wall of the larynx. The cricoarytenoid joints open, close, and tighten the vocal cords during speaking and breathing. Abnormalities can contribute to sleep apnea in people with rheumatoid arthritis.
Genetic factors, exposure to certain environmental conditions, other comorbidities, and lifestyle choices or behaviours, such as a less-than-optimal diet (e.g., too much sugar or fat), heavy drinking or smoking, and insufficient exercise may also be contributing factors.
It was also suggested that the known association between cardiovascular disease and rheumatoid arthritis may, in part, be due to sleep apnea. Obstructive sleep apnea has been tied to inflammation, coagulation, and endothelial dysfunction. As contributing factors have been identified, the cause and effect become more apparent and the need for managing each factor is obvious.
The factors must be considered from the perspective of how rheumatic diseases are related to sleep apnea. For example, it has been determined that people with obstructive sleep apnea have elevated acute-phase reactants (CRP, sedrate) and pro-inflammatory cytokines. It has been reported that some interleukins, specifically, IL-1, IL-2, IL-6, Il-8, IL-18, and TNF-alpha promote non-REM (rapid eye movement) sleep. IL-4, IL-10, IL-13, and TNF-beta inhibit non-REM sleep.
Inflammatory cytokine levels are proportionate to the severity of sleep apnea. Higher levels of TNF-alpha have been associated with more severe obstructive sleep apnea and hypoxia. This may explain why people with rheumatoid arthritis who are treated with TNF blockers find that their fatigue level improves. More study would be needed to draw a conclusion regarding the impact of specific rheumatoid arthritis treatments.
How Should It Be Managed?
The association of rheumatoid arthritis and sleep apnea may significantly contribute to increased morbidity and mortality in people who have both conditions. That the association may contribute to the increased risk of cardiovascular disease in rheumatoid arthritis patients is perhaps most noteworthy.
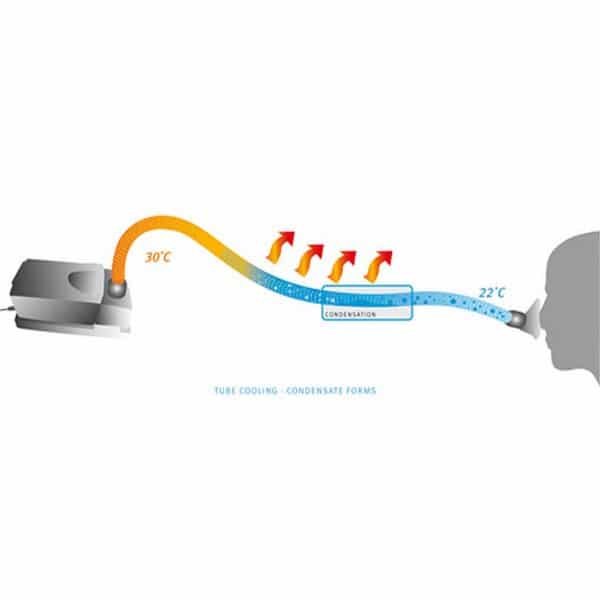
Rheumatologists should look for signs of sleep apnea in their patients when interviewing and evaluating them and, if indicated, refer to a sleep specialist or sleep clinic. Sleep apnea is typically managed by utilizing CPAP devices. Compliance with CPAP devices is a problem for some though. It might be best described as cumbersome. Other possible means for the management of sleep apnea involve specific body position during sleep to keep the airway open, weight loss, and the use of devices to move the mandible forward thereby reducing airway obstruction. For certain, the problem should not be ignored.
The Bottom Line
When someone with rheumatoid arthritis complains to their doctor about fatigue, it should not initially be dismissed as a common characteristic associated with the disease. It should not be assumed that fatigue is simply related to sleep disruption and sleep fragmentation associated with pain. While that may be true in most cases, the hard work of determining the cause must be undertaken. Sleep apnea must be ruled in or out. The potential consequences of untreated sleep apnea are too great otherwise.
Sources:
Ataka, H. et al. Occipitocervical Fusion Have Potential to Improve Sleep Apnea in Patients With Rheumatoid Arthritis and Upper Cervical Lesions. Spine. 2010 Sept 1;35(18):E971-5.
Shen, Te-Shun et al. Risk of Obstructive Sleep Apnoea in Patients With Rheumatoid Arthritis: A Nationwide Population-Based Retrospective Cohort Study. BMJ Open. 2016; 6(11): e013151.
Shoda, Naoki et al. Sleep Apnea in Rheumatoid Arthritis Patients With Occipitocervical Lesions: The Prevalence and Associated Radiographic Features. European Spine Journal. 2009 June; 18(6): 905-910.
Strohl, Kingman P MD. Overview of Obstructive Sleep Apnea in Adults. UpToDate. Updated June 24, 2016.
Taylor-Gjevre, Regina M., Nair, Bindu V., and Gjevre, John A. Obstructive Sleep Apnoea in Relation to Rheumatic Disease. Rheumatology (2013) 52(1):15-21.


































 Got a
Got a




 Travel Tips When Flying or Traveling with
Travel Tips When Flying or Traveling with