Winter can be a challenging time for CPAP users. The lack of humidity in the dry cold winter air, combined with the use of CPAP therapy can cause the nasal passages to become dry while using CPAP with a cold or flu can only make matters worse.
One of the main functions of the nose is to warm and moisten the air you breathe. If the air is cold tiny blood vessels inside the nostrils, dilate to help warm up the air, but the extra blood flow causes the airway to narrow and leads to additional mucus production to protect its sensitive tissues and to add more moisture to the inhaled air. Unfortunately, this may cause nasal congestion and a runny nose.
If the air through the mask does feel too cold and your sleep is disrupted there are some simple remedies that can be tried to overcome this:
- Try closing the windows and heating the bedroom.
- Also try placing the tubing under the bedclothes as heat from the body will increase the temperature of the air passing through it.
- Use the specific humidifier for your CPAP machine.
- Use the heated tube, which will improve the climate of CPAP therapy.
-
Prisma Aqua & Heated Tube Combo – Black250,00 €
-
Prisma Aqua & Heated Tube Combo – White250,00 €
-
Product on saleAirSense 11 Climate Control ComboOriginal price was: 255,00 €.193,10 €Current price is: 193,10 €.
-
Prisma Line Heated Tube, Löwenstein Medical115,00 €
-
Product on saleAirSense 10 Climate Control ComboOriginal price was: 177,00 €.168,10 €Current price is: 168,10 €.
-
Product on saleClimateLineAir 11 Heated Tube for AirSense 11, ResMedOriginal price was: 99,00 €.78,00 €Current price is: 78,00 €.
-
HYBERNITE Heated Tube115,00 €
-
Product on salePrisma Aqua Humidifier white, Löwenstein MedicalOriginal price was: 185,00 €.135,00 €Current price is: 135,00 €.
-
HU Waterless Humidifier Filter, BMC Medical
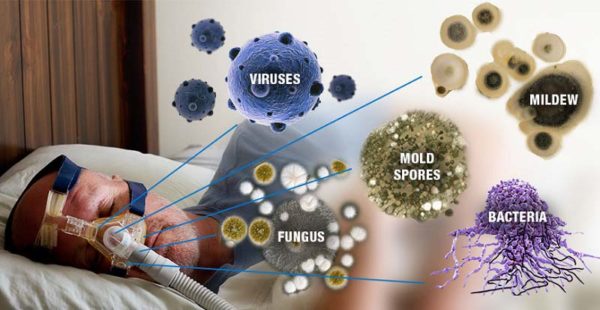
Upper respiratory tract infections, colds and flu
It’s never easy to sleep when you have an upper respiratory tract infection, a cold or flu, but for people on CPAP therapy, it is more difficult to tolerate treatment at this time.
Stopping using your CPAP when you have a cold is not advised as it can make other cold symptoms such as a sore throat a lot worse. However, if you are too uncomfortable or if you experience ear pressure or pain or have any other concerns, contact your GP or medical provider.
Again some simple remedies can be tried to make treatment more comfortable when you do have a cold.
- Use of a saline nasal spray to add moisture to the sinus passages can relieve swelling and help you breathe easier.
- Decongestants can help although these can take a while to work, so they need to be used early enough so that they take effect by bedtime.
- An ‘over the counter spray’ such as Beconase can be used to decrease inflammation in the nasal passages and help reduce the swelling of the nasal mucosa. This is only recommended for short term use, i.e. less than three days. If you are taking any other medicines, including those bought without a prescription and herbal medicines, you should check with your pharmacist before you start treatment with this.
Under no circumstances be tempted to add Olbas oil or similar decongestants to the water in your humidifier and do not put it on the filter of your device as this can damage your equipment.
Use a Full Face CPAP Mask
Most CPAP masks are nasal masks so require you to breathe only through your nose, but when nasal congestion develops, it becomes difficult to do this. Nasal congestion or resistance as experienced during a cold can lead to you breathing through your mouth. When air from your CPAP device escapes through your mouth (mouth leak), it can be a significant problem that may compromise the effectiveness of your CPAP therapy. Mouth leak causes high airflow in one direction, preventing the lung’s moist air from passing back through the nose which results in drying of the skin in the nose, nasal congestion, and flu-like symptoms upon awakening.
Many people who routinely use nasal masks with their CPAP treatment purchase a Full-Face CPAP mask for use when they have a cold or an upper respiratory tract infection. Use of this type of mask will ensure that if you do revert to breathing through your mouth treatment can still be used, and it will continue to be effective.
Add heated humidification
Use of heated humidification with CPAP treatment is recognised as the most effective method of preventing or reversing the symptoms resulting from cold air or an upper respiratory tract infection as the air is warmed and moistened before it reaches the nose. This will help with nasal congestion, ease inflamed nasal passages and make the air more comfortable to breathe.
Some people using heated humidification can experience a problem known as ‘rainout’ during cold weather when the warmed moistened air coming from the humidifier is cooled by room air as it moves down the tube towards the mask and moisture in the cooler air returns to a liquid.
This can result in droplets of water or condensation to gather in the tube and mask.
There are several ways to lessen the problem of ‘rainout’, and the following may help:-
- Always have the device and humidifier positioned lower than the bed.
- Close the bedroom window, turn the humidifier down or raise the temperature in the bedroom at night to lessen the difference between the temperature in the room and the tube.
- Tuck the tube under the bedclothes to keep it warm.
- Insulate the hose by covering it with a tubing wrap.